Gurjeet Jutley has been treating patients suffering with cataracts for many years and in this blog, Gurjeet explains how to spot the symptoms of cataracts and the actions you should take.
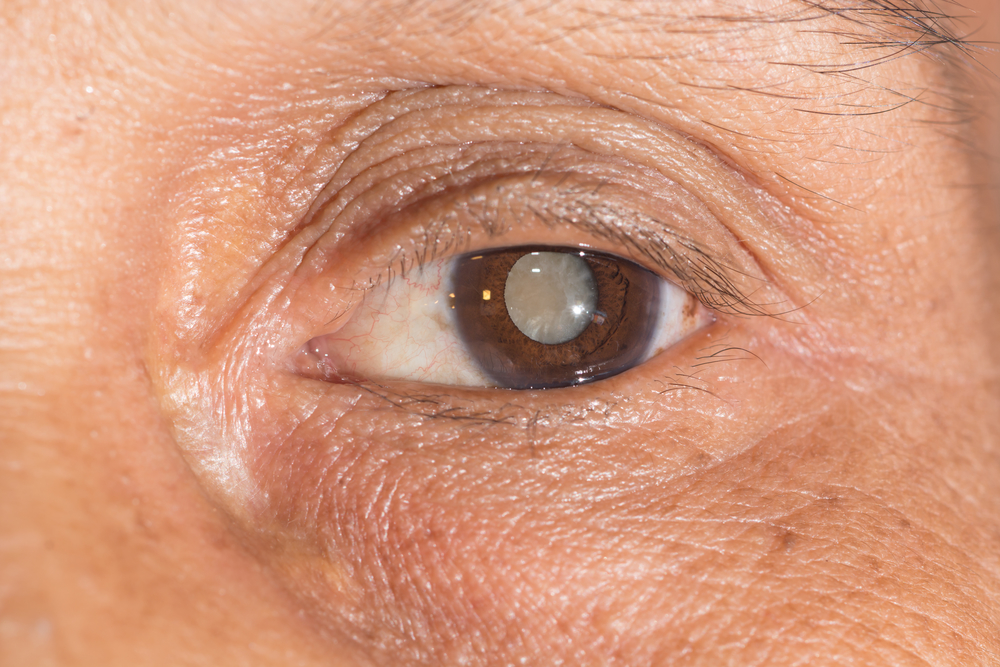
Cataracts involve the lens of the eye developing cloudy patches. These patches can become larger over time, resulting in blurred vision and blindness. As we age, our lenses become more frosted, and our vision is affected. In most cases, cataracts develop in both eyes. However, this is not always at the same pace for each eye, and the condition can develop faster in one eye than the other. If you do develop cataracts, you may find it more difficult to conduct day-to-day activities including reading, driving, watching television and more. Although cataracts are heavily associated with older people, they can even affect young children and babies.
Am I suffering from cataracts?
You may have cataracts if colours have started to seem faded, you cannot see clearly in low light conditions, lights appear brighter than usual or your eyesight has become misty or blurred. Other symptoms can include seeing double. Spectacle wearers may even think their glasses need cleaning when they don’t.
Have you been forced to change your glasses or contact lens prescription more frequently over recent years? If so, this may be a symptom of cataracts. Cataracts aren’t always painful at first. They won’t redden your eyes or make them irritated initially, though they can be more painful when they reach an advanced stage, or if you also have another eye condition.
What happens during testing?
If you are tested for cataracts, a visual acuity exam will be carried out. This exam will assess how well you are able to see at various different distances. You could be referred to an eye specialist if your optician suspects you do have cataracts. More tests will be carried out after this stage. You may be able to wear stronger glasses or use brighter lights for reading if your cataracts are not at an advanced stage. If or when they do get worse, you may need surgery so that the lens can be removed and replaced.
Can I still drive if I have cataracts?
You are expected to inform the DVLA if you develop cataracts in both of your eyes. You don’t need to let them know if you only have cataracts in one eye unless you drive as part of your job or have a medical condition in your other eye. People that drive lorries, coaches or buses are obliged to let the DVLA know even if they only have cataracts in one of their eyes. Cataracts are linked to a range of causes, and these include eye injuries, a family history of the condition, diabetes, smoking, long-term steroid use and excessive alcohol consumption.
What happens during surgery?
If you do need cataract surgery, your surgeon will explain each stage of the treatment to you. Most treatments are carried out under local anaesthetic, and the cloudy lens will be replaced with a synthetic intraocular lens (IOL) to last for the rest of your life. Refractive cataract surgery is another option. With this treatment, the lens is replaced and errors like short and long-sightedness and astigmatism can be corrected. If you undergo this treatment, you may not need to wear your glasses so much – and could be able to stop using them completely.
To find out more, contact Gurjeet Jutley today.
Comments
Post a Comment